-
-
Featured Care Areas

Sinusitis (Sinus Infection)
What is sinusitis?
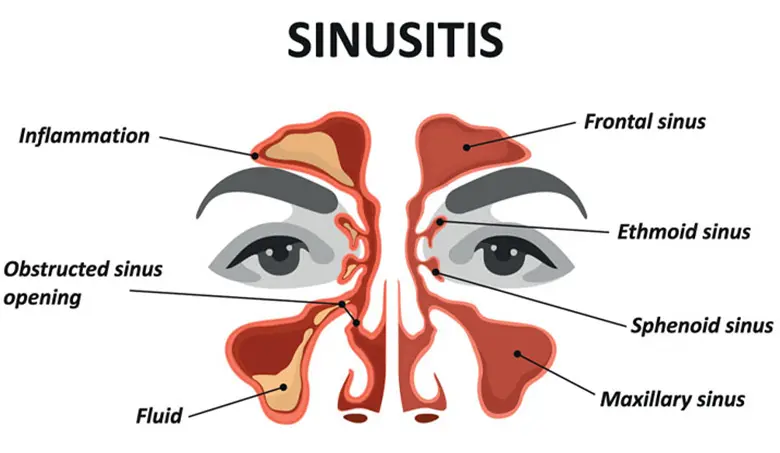
Sinusitis is a disease characterised by inflammation of the tissue lining the sinuses. It can affect people of all ages, including children.
Paranasal sinuses are hollow spaces in the bones of the face and skull that are covered in a thin layer of mucosa (soft tissue lining that produces mucus). The sinuses are connected by narrow pathways to the nasal passages.
Healthy sinuses produce mucus that moisturise the inside of the sinuses and nasal passages. This helps to humidify and warm the air we breathe, and clear micro-organisms and pollutants from our nasal passages.
When sinusitis occurs, the mucosal lining becomes inflamed and swollen, and produces a much larger amount of inflammatory mucus. This inflammation can lead to:
- Congestion and discomfort in the sinuses (often described as facial pain)
- Nasal discharge (often discoloured) or obstruction
- Decreased sense of smell
Types of sinusitis
In general, there are 3 types of sinusitis:
Acute sinusitis
Acute sinusitis, also known as acute rhinosinusitis, can last up to 4 weeks. It can be classified into:
- Viral rhinosinusitis – A condition also known as the common cold, where symptoms typically start to improve after 5 – 10 days.
- Acute bacterial rhinosinusitis – A condition that usually occurs when the common cold does not improve and lasts for many weeks.
Chronic sinusitis
Chronic sinusitis is also known as chronic rhinosinusitis (CRS). The change from acute to chronic sinusitis is a gradual process of persisting sinus inflammation. Symptoms must be present for at least 12 weeks.
CRS can be broadly classified into 2 types, with possible overlapping of features:
- CRS without nasal polyposis (CRSwoNP)
- CRS with nasal polyposis (CRSwNP) – Nasal polyps represent severe swelling of the sinus mucosa. CRSwNP is usually caused by an underlying immune dysfunction that leads to an excessive inflammatory response. The chronic buildup of symptoms typically causes a loss of smell, and sometimes facial pain.
Fungal sinusitis
Fungal sinusitis may be caused by fungal organisms in 3 ways:
- Fungal “ball” or fungal mycetoma – The most common type of fungal sinusitis which usually affects just one sinus. The fungus grows within the sinus, causing localised inflammation.
- Allergic fungal rhinosinusitis (AFRS) – A condition that usually affects multiple sinuses on both sides, with marked swelling of the sinus mucosa (polyposis) and thick allergic mucus discharge. AFRS usually occurs in younger people with a history of nasal allergies.
- Invasive fungal sinusitis (IFS) – A severe and potentially fatal condition that usually occurs in immunocompromised patients, such as diabetes mellitus patients on immunosuppressive treatment. The fungus causes destruction of tissues in and around the nose and sinuses.
What are the symptoms of sinusitis?
The symptoms of sinusitis include:
Nasal obstruction
- Difficulty breathing through the nose due to blockage
- Mouth breathing
- Snoring
Sinus congestion
- Feeling full in the face
Nasal discharge
- Thick and yellow or green discharge
Postnasal drip
- The sensation of mucus in the back of the throat
- Cough with phlegm but sometimes even “dry” cough
- Bad breath
Facial pain
- Feeling heavy in the head
- Pain around the eyes, nose, cheeks and forehead
In addition, you may experience a reduced sense of smell and taste, tiredness, fever or a sense of general malaise.
When to seek medical attention?
In general, you should consult an ENT specialist if you have the following symptoms:
- Loss of smell
- Persistent sinusitis (e.g. for more than 1 month)
- Recurrent sinus infections (e.g. more than 4 times per year)
- Blood-stained nasal discharge
If you experience any of the following symptoms, you should consult an ENT specialist immediately, as they may suggest severe complications of sinusitis (e.g. infection spreading to the eyes or brain):
- Fever above 38°C
- Blurred or double vision
- Swelling and redness around the eyes
- Severe facial pain or headaches
- Stiffness in the neck
- Mental confusion
What causes sinusitis?
Sinusitis is usually due to a combination of factors acting at the same time, often triggered by a viral upper respiratory tract infection that predisposes you to secondary bacterial infection and impaired clearance of inflammatory mucus.
These factors include:
Anatomical abnormalities of the nose
Examples of structural abnormalities include a deviated nasal septum that may narrow the outflow tract of the sinuses.
Uncontrolled allergic rhinitis
Untreated allergic rhinitis (allergic inflammation of airways in the nose) is one of the factors that can lead to sinusitis.
Dental infections
Dental infections such as tooth infections usually cause isolated maxillary sinusitis.
Deficiences in immune function
If you have a weakened immune function, fungal sinusitis, viral infections and bacterial infections may lead to sinusitis.
What are the risk factors for sinusitis?
Risk factors for sinusitis include:
Nasal polyps
Nasal polyps are painless, soft and non-cancerous growths on the nasal passages or the lining of your sinuses.
Asthma
People with asthma are prone to developing sinusitis. This is because asthma causes the airways to narrow and swell, which may produce extra mucus and result in breathing difficulties. Asthma may also trigger coughing, wheezing and shortness of breath.
Pollutants
Regular exposure to pollutants such as tobacco smoke can trigger sinusitis.
Other medical conditions
Health conditions like HIV, cystic fibrosis and other immune system-related diseases can lead to nasal blockage, which increases your risk of sinusitis.
What are the complications and related diseases of sinusitis?
While sinus infection is generally not life-threatening, it can lead to complications if left untreated. These complications include:
Eye infection and abscess
Sinus infection can spread to the eyes. In the early stages, the eyelids may become swollen. As the infection progresses, the eye itself becomes swollen and painful. The structures of the eye may be damaged and result in vision problems such as double vision or blindness.
Blood clot in the cavernous sinus
Untreated sinusitis may lead to blood clots in the cavernous sinus (an important venous system at the base of the brain). These blood clots can:
- Restrict blood flow from the brain
- Allow bacteria to spread through the bloodstream, leading to brain tissue injury and eye tissue injury.
Brain infection – meningitis and brain abscess
Infection of the sinuses may spread to the meninges (membranes surrounding your brain). Classic symptoms of a meningeal infection include high fever, headache and neck stiffness, and altered neurological function.
Further bacterial spread can lead to the formation of brain abscesses (accumulation of pus and breakdown products from infection). The swelling and pressure of the brain tissue can cause neurological deficits and coma.
Bone infection – osteomyelitis
The bacterial infection from the sinuses may spread to the surrounding bone, especially the bone of the forehead. This can lead to persistent headache, fever, swelling of the bone and discharge of pus through the skin.
How do you prevent sinusitis?
You can prevent sinusitis by:
- Not smoking and avoiding secondhand smoke
- Keeping your hands clean, especially during cold and flu season
- Avoiding close contact with people with upper respiratory infections or colds
- Being aware of your allergies and avoiding triggers
- Getting flu and pneumococcal vaccinations
This page has been reviewed by our medical content reviewers.
Need help?
For enquiries, please call
+65 6377 3737
For appointment bookings, please WhatsApp
+65 8111 3777