-
-
Featured Care Areas

Pelvic Organ Prolapse (POP)
What is pelvic organ prolapse (POP)?
Pelvic organ prolapse (POP) occurs when the pelvic organs drop from their original position in the pelvis. It is a very common condition, especially among older women.
The condition occurs when the pelvic floor muscles are weak or damaged, and can no longer support the organs of the pelvis. POP can involve any of the pelvic organs, including the:
- Uterus (womb)
- Ovaries
- Fallopian tubes
- Rectum
- Bladder
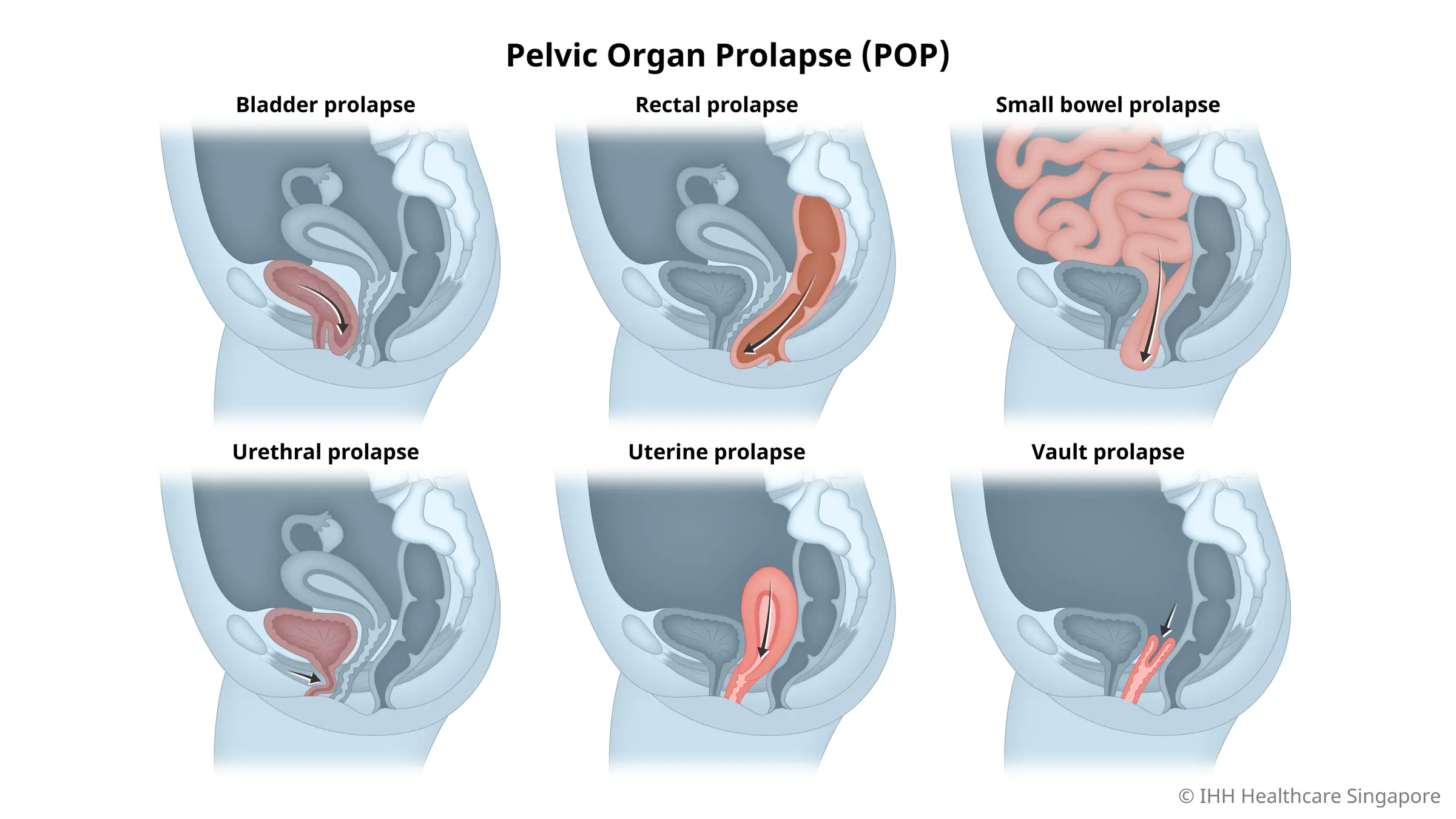
Types of pelvic organ prolapse (POP)
There are several types of POP:
Bladder prolapse
Also called anterior prolapse or cystocele, a bladder prolapse occurs when the wall located between your bladder and vagina stretches and weakens.
The weakening of this wall causes the bladder to droop down and press into your vagina. This may cause you to feel a constant urge to urinate and experience problems with emptying your bladder, such as urinary retention.
Rectal prolapse
Rectal prolapse is also called posterior vaginal prolapse or rectocele. The condition occurs when the fascia (the fibrous tissue that serves as a wall to separate the rectum from the vagina) weakens, creating a bulge in your vaginal wall.
Various conditions can increase your risk of developing a rectal prolapse, primarily those that can cause pressure on your pelvic floor like chronic constipation, chronic cough, pregnancy and childbirth.
Although small bulges may not show any symptoms and rarely cause any pain, it is still important to have it checked by your doctor, especially when the bulge becomes more prominent and uncomfortable.
Small bowel prolapse
Small bowel prolapse, or enterocele, is a form of POP in which the small intestine descends into your lower pelvis and presses at the top portion of your vagina, forming a bulge.
A mild to moderate small bowel prolapse may not produce any signs and symptoms, and most often, the only way to know that you have the condition is to go for a pelvic examination.
Urethral prolapse
Urethral prolapse is also known as urethrocele. The condition occurs when the urethra (the tube that transports urine from the bladder to the outside of the body) descends and prolapses into your vaginal canal.
When the muscles and tissues that support your urethra are damaged due to pregnancy, prolonged labour or menopause, the urethra widens, causing it to curve downward and press into your vagina.
Just like a bladder prolapse, urethrocele can cause urination problems, such as difficulty passing urine and completely emptying your bladder.
Uterine prolapse
Just like other forms of POP, uterine prolapse is caused by conditions and activities that pressure your pelvic floor.
When there is excessive pressure on your pelvis, the muscles and tissues that hold the uterus in place become weak. This allows the uterus to slip from its normal position and bulge down into your vagina or birth canal.
Uterine prolapses can be categorised into the following grades:
- Grade 1 – The uterus has dropped slightly and may not be noticeable. There are no symptoms.
- Grade 2 – The uterus has dropped further into the vagina and the cervix (neck or tip of the womb) can be seen at or just outside the vaginal opening.
- Grade 3 – A large portion of the uterus has fallen through the vaginal opening.
- Grade 4 – The whole uterus has fallen through the vaginal opening (procidentia).
Vault prolapse
The vagina collapses in on itself after a hysterectomy (surgical womb removal).
What are the symptoms of pelvic organ prolapse (POP)?
Symptoms of POP include:
- Backache that progresses through the day.
- A dragging sensation in the lower abdomen and pelvis.
- A swelling sensation in the vagina or a lump outside the vagina.
- Vaginal bleeding and discharge (not part of the menstrual cycle).
- Difficulty in or inability to have sex, which may cause anxiety or depression.
- Difficulty in passing urine or stools.
- Difficulty in walking or sitting.
What causes pelvic organ prolapse (POP)?
A prolapse is caused by the continuous weakening of the supporting tissues of the pelvic organs. This weakening may be caused by:
- Collagen deficiency.
- Chronic cough or strain from constipation.
- Congenital (present at birth) weakness of the pelvic floor muscles, ligaments and fascia.
- Menopause, where the supporting tissues become weaker with age and menopause.
- Pregnancy and childbirth, especially after a difficult and prolonged labour.
- Obesity, large fibroid (fibrous growth), tumour or previous pelvic surgery.
- Strenuous physical work or heavy lifting.
What are the complications and related diseases of pelvic organ prolapse (POP)?
In general, POP is not a life-threatening condition. However, some cases can result in the following complications:
- Bedwetting
- Difficulty in urinating
- Urinary tract infections
- Urinary incontinence or bladder control problems
- Pain around the vulva and vestibule in women
- Hydronephrosis and kidney damage
- Prostate inflammation (in men)
- Pain during sexual intercourse
- Bowel control
- Constipation
Treatments for pelvic organ prolapse may also cause some complications. For example, a pessary (a removable device placed in the vagina) can cause vaginal discharge, vaginal bleeding and ulcers in the vaginal epithelium.
Likewise, while complications are rare after surgery for POP, the treatment also comes with the risk of complications like infection, bleeding and pelvic organ damage.
This page has been reviewed by our medical content reviewers.
Need help?
For enquiries, please call
+65 6377 3737
For appointment bookings, please WhatsApp
+65 8111 3777