-
-
Featured Care Areas

Ulcerative Colitis
What is ulcerative colitis?
Ulcerative colitis is a type of inflammatory bowel disease that affects the innermost lining of the large intestine (colon) and rectum.
Patients with this condition have chronic inflammation of the colon and ulcers that gradually worsen, and can bleed and produce pus.
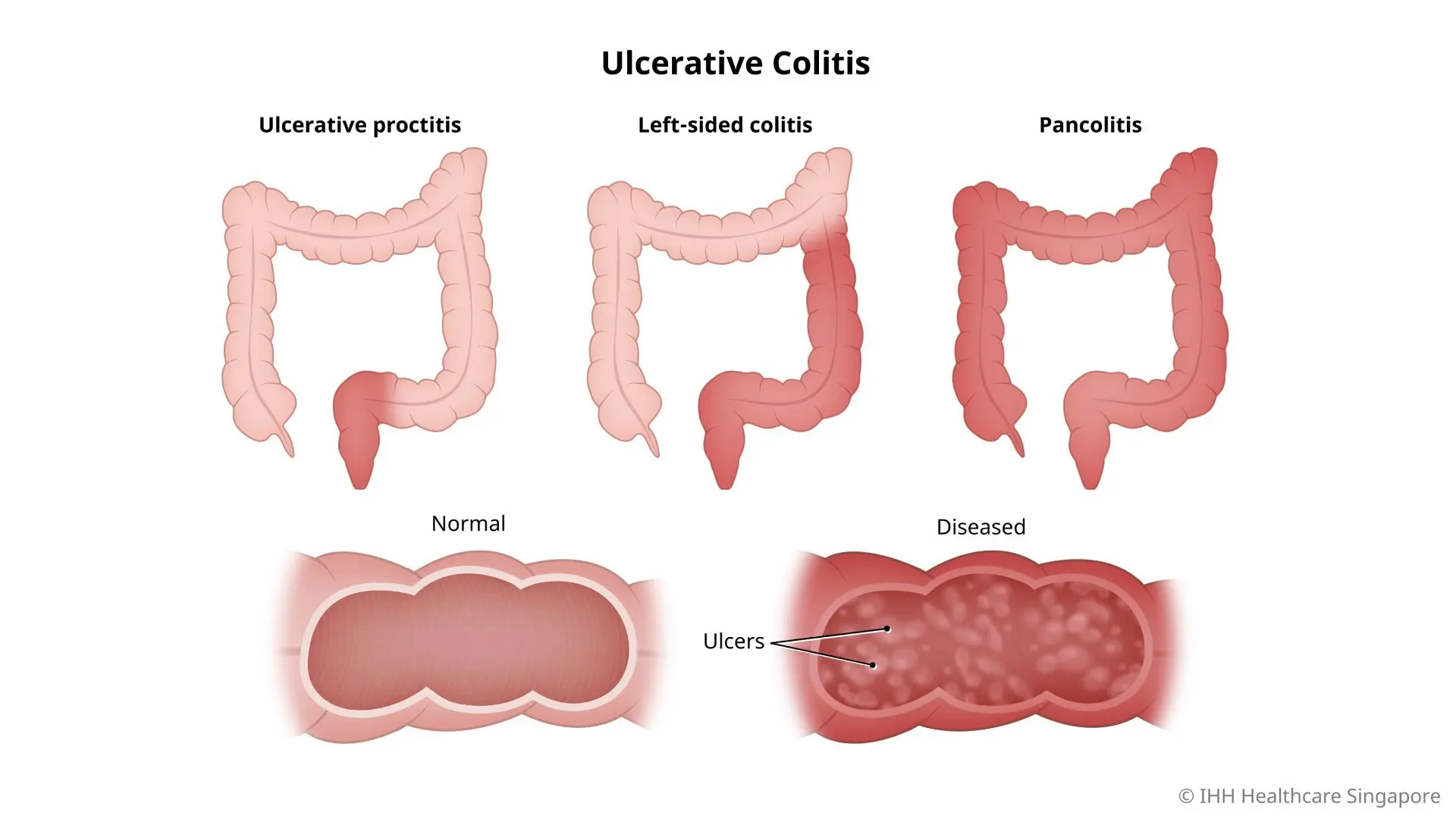
Types of ulcerative colitis
There are 3 types of ulcerative colitis depending on its location:
- Ulcerative proctitis. This is the mildest form where inflammation is confined to the rectum. Rectal bleeding is usually the only sign of the disease.
- Left-sided colitis. This involves inflammation from the rectum extending further into the colon. Symptoms include bloody diarrhoea, pain and cramping in the left side of the abdomen, and significant weight loss.
- Pancolitis. This involves inflammation of the entire colon. Symptoms include bloody diarrhoea that is severe, pain and cramping in the abdomen, fatigue, and significant weight loss.
Ulcerative colitis can weaken your body. There is no cure for this condition yet. However, with careful treatment, you can have periods of remission with no symptoms.
What are the symptoms of ulcerative colitis?
Ulcerative colitis symptoms vary depending on the severity and location of the inflammation. They include:
- Abdominal pain and cramping
- Pain and bleeding in the rectum
- Recurring diarrhoea with blood or pus
- The urgency to pass stools but an inability to do so
- Extreme tiredness, loss of appetite, and weight loss
- Fever
Most people have mild to moderate symptoms. Some patients may have weeks to months of mild symptoms or absence of symptoms, followed by flare-ups or relapses. Symptoms of a flare-up include:
- Mouth ulcers
- Shortness of breath and a fast or irregular heartbeat
- Painful and swollen joints (arthritis)
- Painful, red, and swollen skin
- Irritated and red eyes
- More blood in stools
- Fever
What causes ulcerative colitis?
The exact causes of ulcerative colitis remain unknown. Possible causes that have been suggested include:
- Immune system malfunction. An abnormal immune response may cause the immune system to attack its own digestive tract cells.
- Heredity. Ulcerative colitis is more common in people who have family members with the disease.
What are the risk factors for ulcerative colitis?
Factors that may increase your risk of developing ulcerative colitis include:
- Age. Ulcerative colitis commonly develops in people under the age of 30 and over 60.
- Ethnicity. Ulcerative colitis is more common among people of European descent and rare in people from Asian backgrounds.
- Family history. Having a close family member with the disease increases your risk.
What are the complications and related diseases of ulcerative colitis?
There are several possible complications related to ulcerative colitis, including:
- Inflammation of the skin, joints, and eyes.
- Damage to the colon, such as severe bleeding, tearing or perforation of the colon.
- Severe dehydration, as the inflamed intestines cannot absorb fluids effectively.
- Osteoporosis (bone loss). This can develop due to prolonged use of corticosteroids or from dietary changes such as avoiding dairy products.
- An increased risk of colon cancer, especially among those who have the severe type of disease or inflammation involving most of the colon.
- Toxic megacolon (rapid swelling of the colon). This is a rare and serious complication of severe ulcerative colitis. In toxic megacolon, colon inflammation traps gas, resulting in an enlarged and swollen colon.
- Blood clots in the veins and arteries.
How do you prevent ulcerative colitis?
Though there is no firm evidence that dietary changes can prevent ulcerative colitis symptoms, you may consider the following dietary lifestyle changes:
- Avoid trigger foods, such as spicy foods, alcohol, and caffeine.
- Limit dairy products. This has been found to help with symptoms such as diarrhoea, abdominal pain, and gas.
- Limit fibre. High-fibre foods such as fruits, vegetables, and whole grains may make symptoms worse in some people. Steaming, baking, or stewing raw fruits and vegetables may help.
- Eat small meals and drink plenty of water. Breaking meals into 5 or 6 small meals throughout the day may be helpful.
- Manage stress by exercising regularly, resting, relaxing, or meditating.
These changes may help you to control your condition (e.g. lengthen the remission period and prevent flare-ups) and get the nutrition you need.
Tip: Keep a food diary to record what and when you eat. This can help you identify and eliminate food items that trigger flare-ups.
This coverage checker is brought to you by Health Insured, an online resource that helps you understand your health coverage in Singapore.
This page has been reviewed by our medical content reviewers.
Need help?
For enquiries, please call
+65 6377 3737
For appointment bookings, please WhatsApp
+65 8111 3777